In vitro fertilization (IVF)
IVF is the most common and effective type of assisted reproductive technology to help people become pregnant. IVF can help achieve pregnancy when other treatments have not worked.
IVF is a treatment for infertility in which a woman’s eggs (oocytes) are fertilized by sperm (her partner’s or donor sperm) in a laboratory dish. The fertilized eggs develop into embryos in the IVF laboratory. One or more of the embryos are then transferred into the woman’s womb.
One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
Who should consider in vitro fertilization?
- Age: Advanced reproductive age, as time to conception is critical and pregnancy rates with other therapies are low.
- Fallopian tube damage or blockage
- Previous tubal sterilization or removal: IVF may be an alternative to tubal ligation reversal surgery in woman who wishes to conceive after tubal ligation.
- Ovulation disorders
- Unexplained infertility: Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- Uterine fibroids
- Pelvic adhesions
- Decreased ovarian reserve or early menopause.
- Abnormal sperm production or function: Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm shape can make it difficult for sperm to fertilize an egg.
- IVF for fertility preservation may be an option if you’re about to start cancer treatment, such as radiation or chemotherapy. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
- Women who don’t have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman’s eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier’s uterus.
- A genetic disorder: Some couples may even carry a known genetic illness and wish to avoid passing this illness on to a child. In special circumstances, a more advanced fertility treatment known as pre-implantation genetic testing (PGT) may be offered in conjunction with IVF. PGT allows the couple to find out genetic information about embryos prior to implanting those embryos in a woman’s body. Embryos that don’t contain identified problems can be transferred to the uterus.
Steps involved in the IVF and embryo transfer process:
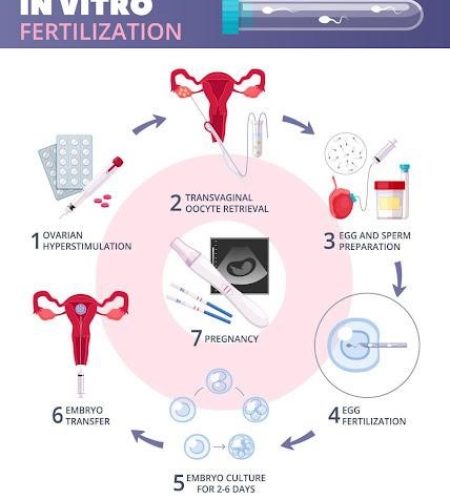
Ovarian stimulation: First you will receive medicines to cause many eggs to grow and mature in your ovaries and to prevent your body from releasing the developing eggs too soon. These medicines are given by injections that are either intramuscular (into the muscle) or subcutaneous (under the skin). You are given appropriate doses of hormone injections containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both once per day for your ovaries to produce 8-10 eggs. When there are ‘leading’ follicles 16mm-20mm in diameter, a different ‘trigger’ injection is given to mature the egg(s). The vast majority of IVF cycles worldwide are performed with some type of ovarian stimulation because natural cycle IVF (IVF without ovarian stimulation, usually only one egg is retrieved) is associated with very low pregnancy rates.
Monitoring: Response to the medicines is monitored by ultrasound and blood tests by measuring the growth of follicles (egg sacs) and rise in hormones respectively. If this monitoring shows that there is likely to be a low chance for successful egg retrieval, the stimulation cycle may be stopped and no egg retrieval will be done.
Triggering: After ovulation induction, another medicine is injected 36 hours before having the egg retrieval procedure to prepare your follicles to mature and release eggs.
Egg Retrieval: The egg collection is a day care procedure under either intravenous sedation or general anesthesia. Most patients are home by lunch time. You are advised to stay home and rest for the two to three days between egg collection and embryo transfer as you will feel uncomfortable.
Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs. If your ovaries aren’t accessible through transvaginal ultrasound, an abdominal ultrasound may be used to guide the needle. The eggs are removed from the follicles through a needle connected to a suction device.
Sometimes IVF cycles need to be cancelled before egg retrieval for one of these reasons:
- Inadequate number of follicles developing
- Premature ovulation
- Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome
- Other medical issues
Egg Fertilization: Your retrieved eggs will be prepared and fertilized in the laboratory using your partner’s (or donor’s) sperm. Sperm is collected from your male partner (or donor) before the egg retrieval. Typically, the semen sample is collected through masturbation. Some men need a needle to remove sperm from the testicles known as testicular aspiration. Donor sperm also can be used if no sperms are found on testicular aspiration.
Fertilization may be tried in one of 2 ways:
Insemination: The eggs are placed in a culture dish and are exposed to sperm that have been washed and processed.
Intra-Cytoplasmic Sperm Injection (ICSI): A single sperm is directly injected into each egg. It may be used when the chances of normal fertilization by the insemination method appear low.
Embryo Transfer
After egg retrieval the development of the embryos is carefully monitored over the next two to five/six days by the embryologist. The best quality embryo or embryos are selected for transfer. The embryos are loaded into a narrow catheter which is passed through the neck of the womb in order to place the embryos, under ultrasound control, near the top of the cavity of the womb. By doing mock transfer before your IVF, potential difficulties can be discovered beforehand. In a mock transfer, we will insert a soft catheter into your uterus to mimic the actual embryo transfer.
After-Transfer Management
You will receive Hormonal medicines to support attachment of embryos to the wall of the uterus to achieve pregnancy and early embryo growth. After the embryo transfer, you can resume your usual daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity.
Results
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you’re pregnant.
Home urine pregnancy testing is not as sensitive for detecting an early pregnancy as blood testing.
If the first blood hCG level is <5 IU/L, the woman is not pregnant.
If the first hCG level is >10 IU/L, the test is usually repeated 48 hours later to confirm that the levels are increasing.
Chances of success with IVF
Each couple has a unique set of circumstances, and the chances of treatment success vary widely. The chances of giving birth to a healthy baby after using IVF depend on various factors, especially the woman’s age, cause of infertility, treatment approach, the quality of your embryos, and your individual circumstances.
In approximately 30-40% of cases (depending on the woman’s age) the embryos will implant to become a pregnancy.
Benefits of IVF
- Pregnancy
- Additional embryos may be cryopreserved for your future family building.
What are the options for extra embryos created from IVF?
If your IVF procedure results in too many embryos (more than the number selected for transfer), the extra ones may be cryopreserved, depending on their quality.
What are the possible risks and complications from this treatment?
Although IVF has a high rate of success in helping couples to become pregnant, it has some disadvantages as well.
- High costs
- Multiple births – IVF increases the risk of multiple births if more than one embryo is transferred to your uterus.
- Premature delivery and low birth weight.
- Ovarian hyperstimulation syndrome (OHSS) – It is a condition in which the side effects of ovarian enlargement and abdominal swelling become extreme. The woman may develop severe abdominal pain, vomiting, and if untreated, blood clots in the legs or lungs and fluid imbalances in the blood. Mild forms of OHSS occur in 2 to 6 percent of women undergoing ovulation induction for IVF. Severe cases of OHSS occur in approximately 1 percent of cases, typically in association with the retrieval of more than 20 eggs. The IVF cycle may be cancelled before hCG is given or after the oocyte retrieval to reduce risk of OHSS. If the cycle is cancelled after oocytes are retrieved, they are often fertilized and cryopreserved (freeze all embryos) for use in a subsequent cycle.
- Egg-retrieval procedure complications -Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel.
- Ectopic pregnancy
- It can be difficult to deal with the emotional highs and lows of infertility treatment.
